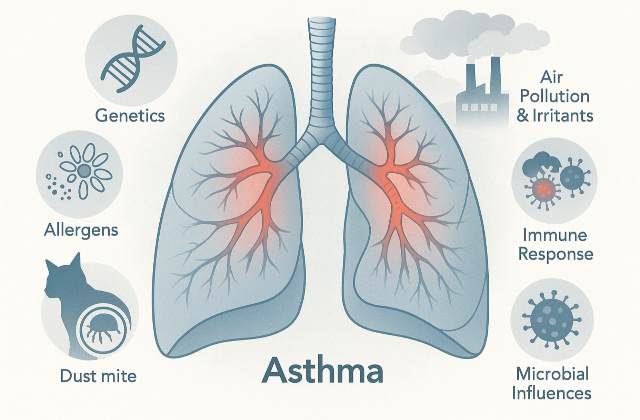
Asthma is a chronic inflammatory disorder of the airways characterized by episodic bronchoconstriction, airway inflammation, and mucus hypersecretion. During an asthma attack, the airways narrow significantly, leading to symptoms such as wheezing, coughing, shortness of breath, and chest tightness. Although asthma can begin at any age, it often starts in childhood and affects hundreds of millions of people worldwide. The causes of asthma are multifactorial, with the condition arising from a complex interplay between genetic predispositions, environmental exposures, immunologic mechanisms, and other contributing factors.
Genetic Factors and Inherited Predisposition
Family history is one of the strongest risk factors for developing asthma. Children born to parents—particularly mothers—with asthma or other allergic conditions are at a higher risk. Twin studies indicate that if one identical twin has asthma, the other’s risk can be dramatically increased. Researchers have identified more than 100 genes related to immune regulation, inflammation, and lung function (e.g., IL4, IL4R, ADAM33) that contribute to asthma susceptibility. It is important to note, however, that having a genetic predisposition does not guarantee the development of asthma; the interaction of these genes with various environmental exposures often determines the ultimate clinical expression of the disease.
Moreover, recent research on epigenetic modifications suggests that changes in gene expression—in response to environmental factors such as lifestyle, diet, and microbial exposure—may further influence asthma development. These heritable changes do not alter the DNA sequence but can impact how genes related to immune response and airway sensitivity are expressed.
Allergens
Allergens are among the most well-documented environmental triggers of asthma. Many individuals with asthma have what is known as allergic, or atopic, asthma in which inhaled substances such as pollen, dust mites, pet dander, mold spores, and cockroach debris lead to an inappropriate immune response.
In these individuals, exposure to an allergen results in the production of immunoglobulin E (IgE) antibodies. These antibodies bind to receptors on mast cells, priming them for an immediate response. Upon subsequent exposure, cross-linking of the bound IgE molecules triggers mast cell degranulation, leading to the release of histamine, leukotrienes, and other inflammatory mediators that cause the airways to spasm and produce excessive mucus, thereby narrowing the airways.
Air Pollution and Chemical Irritants
Air pollutants—including particulate matter from vehicle exhaust, industrial emissions, smog, and nitrogen dioxide—have been strongly linked to the onset and exacerbation of asthma. These outdoor pollutants can inflame the airways, making them more reactive to other triggers. Indoor chemical irritants, such as volatile organic compounds (VOCs), formaldehyde, and cigarette smoke, are similarly associated with increased airway inflammation and asthma symptoms.
Tobacco smoke, in particular, not only irritates the airways of active smokers but also significantly affects children and adults exposed to secondhand smoke. The continuous exposure to these irritants can lead to both an acute worsening of symptoms and chronic changes in lung tissue over time.
Occupational Exposures
Many individuals develop or experience worsening of asthma as a result of exposure to hazardous substances in the workplace. Known asthmagens—substances that cause or exacerbate asthma—include chemicals such as isocyanates, metal dust, wood dust, pesticides, and certain cleaning agents. People working in manufacturing, agriculture, or industries where chemical exposures are routine are at a higher risk. Consistent exposure to these irritants can trigger immune responses that lead to chronic airway inflammation and the development of asthma or the exacerbation of preexisting symptoms.
Immunological and Inflammatory Mechanisms
The pathophysiology of asthma is deeply rooted in an abnormal immune response. In allergic asthma, when an individual inhales an allergen, antigen-presenting cells (like dendritic cells) process and present allergen peptides to naïve T-helper cells. This process encourages the differentiation into TH2 cells, which secrete cytokines such as IL‑4, IL‑5, and IL‑13.
These cytokines stimulate B cells to produce IgE, which coats mast cells through high-affinity receptors. Upon re-exposure to the allergen, these mast cells rapidly release inflammatory mediators, including histamine and leukotrienes. The release of these substances not only causes immediate bronchoconstriction but also sets off a cascade that recruits eosinophils, neutrophils, and other inflammatory cells to the airways, thereby sustaining chronic inflammation. Over time, these inflammatory processes can lead to structural changes in the airway—a process known as airway remodeling—that may reduce reversibility and impair lung function.
Microbial Infections and the Hygiene Hypothesis
Viral respiratory infections, such as those caused by respiratory syncytial virus (RSV) or human rhinovirus, are recognized as important triggers for asthma, particularly in early childhood when the respiratory system is still developing. Such infections can cause significant inflammation and injury to the airways, setting the stage for chronic reactive changes later in life.
In contrast, the hygiene hypothesis proposes that decreased exposure to a diverse range of microbes during early childhood—due to modern sanitation practices, smaller family sizes, and urban living—may lead to an imbalance in immune system development. Specifically, this lack of microbial stimulation may skew the immune response toward a TH2-dominant (allergic) profile rather than a balanced TH1/TH2 response, thereby increasing the risk of developing asthma. Additionally, atypical pathogens such as Chlamydia pneumoniae and Mycoplasma pneumoniae have been implicated in the chronic inflammation observed in some asthmatic patients.
Lifestyle Factors and Additional Influences
Lifestyle choices further contribute to both the development and severity of asthma. Active smoking and exposure to secondhand smoke are well-established contributors to chronic airway inflammation. Obesity is another significant risk factor, as excess weight can impose mechanical restrictions on lung expansion and is associated with a state of low-grade systemic inflammation, both of which can exacerbate asthma symptoms.
Psychological stress also plays a role; it can modulate immune system function and heighten airway responsiveness to triggers. Additionally, diets low in antioxidants and high in processed foods may contribute to increased oxidative stress and inflammatory responses in the airways.
Special Asthma Phenomena
Certain environmental phenomena can trigger severe, even mass, asthma exacerbations. One such phenomenon is “thunderstorm asthma,” which occurs when thunderstorms during high-pollen seasons cause pollen grains to rupture into finer particles. These tiny fragments can penetrate deep into the lower airways and provoke sudden, severe asthma attacks. Such events have led to spikes in emergency room visits and, in some cases, fatalities. This phenomenon underscores the importance of understanding not just the usual triggers but also episodic environmental events in the management of asthma.
Interactions Between Multiple Factors
Asthma rarely arises from a single cause. Instead, the onset and severity of the disease result from the interplay of numerous factors—genetic predisposition, environmental exposures, immune dysregulation, and lifestyle influences. For example, a child with a genetic susceptibility who grows up in an environment rich in allergens and exposed to pollutants may have an overactive immune response that, when compounded by occasional respiratory infections, leads to chronic airway inflammation and even structural changes in the lungs. Recognizing and dissecting these multifactorial interactions is critical for devising effective prevention and treatment strategies.
Synthesis and Outlook
The complex origins of asthma reflect how genetic, environmental, immunologic, and lifestyle factors converge to create chronic airway inflammation and hyperresponsiveness. Genetic predispositions—especially when coupled with early-life exposures to allergens, pollutants, and infections—establish the foundation for an overreactive immune response. Subsequent exposures and lifestyle choices, such as smoking and stress, further exacerbate this condition, often resulting in airway remodeling and persistent symptoms.
This comprehensive understanding emphasizes that effective management of asthma requires a personalized approach—one that identifies and minimizes individual triggers, combines medical therapy (e.g., inhaled corticosteroids, bronchodilators, and leukotriene modifiers) with lifestyle modifications, and utilizes ongoing monitoring to adjust treatment as necessary. Continuous research into these complex mechanisms is paving the way for innovative and targeted interventions, promising improved outcomes and quality of life for asthma sufferers.
Final Note
While the precise cause of asthma may remain elusive for some individuals, the ongoing research into genetic, environmental, and immunologic factors continues to pave the way for improved interventions and prevention strategies. For patients and caregivers, a combination of good medical care, environmental modifications, and lifestyle adjustments can make a substantial difference in managing the disease and enhancing quality of life.
This multi-layered understanding offers hope—not only for better treatments now but also for eventual strategies that might prevent the onset of asthma altogether.